Rerum cognoscere causas. This phrase translates as ‘to know the causes of things’. It is the basis and impetus of public health. But epidemiologists have a different word for it: causal inference.
Does ‘A’ cause ‘Y’? And how can we be sure that ‘A’ alone caused ‘Y’ and that some other variable didn’t have a hand in this relationship between ‘A’ and ‘Y’? Let’s put this in practical heathcare terms. Does drinking 1-2 glasses of wine per day result in a lower risk of heart disease as compared to people who don’t drink 1-2 glasses of wine per day? Is a little bit of wine beneficial? Or are drinkers of 1-2 glasses of wine more affluent and able to maintain a healthy lifestyle? Do people who get the flu vaccine have a lower mortality rate than those who don’t get vaccinated? Does the vaccine increase survival? Or are those who get vaccinated less sick than those who don’t get vaccinated?
 Here’s another way to look at it. Take a look at Figure 1. Think about it. Do you think the pill caused Ian’s death in Scenario 1? And what about Scenario 2? Most likely you would say that the pill did, indeed, cause Ian’s death in Scenario 1 but did not have an effect on Jim’s survival in Scenario 2. Why is this the case? Because the outcomes are different for Ian in Scenario 1 and the same for Jim in Scenario 2. Simply put, we tend to compare the outcome when an exposure is present versus when it is absent. If the outcomes are different, we say that the exposure has a causative effect. In Ian’s case, the act of taking the pill or not taking the pill resulted in a different outcome. For Jim, the action of taking the pill or not taking the pill resulted in the same outcome.
Here’s another way to look at it. Take a look at Figure 1. Think about it. Do you think the pill caused Ian’s death in Scenario 1? And what about Scenario 2? Most likely you would say that the pill did, indeed, cause Ian’s death in Scenario 1 but did not have an effect on Jim’s survival in Scenario 2. Why is this the case? Because the outcomes are different for Ian in Scenario 1 and the same for Jim in Scenario 2. Simply put, we tend to compare the outcome when an exposure is present versus when it is absent. If the outcomes are different, we say that the exposure has a causative effect. In Ian’s case, the act of taking the pill or not taking the pill resulted in a different outcome. For Jim, the action of taking the pill or not taking the pill resulted in the same outcome.
So, while causal inference, which attempts to explain the effect of an exposure or treatment on an outcome, is the backbone of much of what we do in public health, we often get tripped up by confounding. Confounding is the bias that arises when we make causal inferences based on non-comparable groups. In other words, we can’t have people of different ages, different genders or different baseline health status in different groups and then attempt to draw some meaningful causative conclusion about those two groups. The two groups are, by definition, different. We can say that there is an association between the exposure and the outcome in these groups. But we cannot say that the exposure causes the outcome.
So, we control for potential confounding by conducting randomised controlled trials. Randomised controlled trials make groups the same by virtue of their study design. We don’t worry about the groups being different anymore. Unfortunately, the randomised controlled trial is not always easy to execute because of costs, time, ethical concerns and other issues.
But we still need to make policy decisions. We still need to know whether to treat or not to treat. So, we have to use observational studies and data to guide and inform our approach to disease management. And in using an observational approach, we
must know how to tell whether
a variable is a confounder or not.
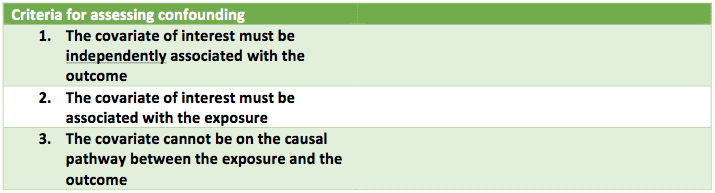 Let’s take a look at a simple example in the observational world: the case of whether age is a confounder for the relationship between coronary heart disease, the exposure, and death, the outcome. For a variable to be considered a confounder, three criteria must be met (see Figure 2). In plain English, this means that
Let’s take a look at a simple example in the observational world: the case of whether age is a confounder for the relationship between coronary heart disease, the exposure, and death, the outcome. For a variable to be considered a confounder, three criteria must be met (see Figure 2). In plain English, this means that
1.
Age must be independently associated with death. And it is. Older people are more likely to die than younger people.
2.
Age must be associated (although not independently) with coronary heart disease.
And it is. Older people tend to have a greater prevalence of heart disease than younger people.
3.
Age cannot be on the causal pathway between coronary heart disease and death. In other words, having coronary heart disease does not ‘cause’ one to age which, in turn, leads one to die.
Our three criteria are met. And, as a result, age is a confounder in our observational study of the effect of coronary heart disease on the risk of death.
Why am I bothering to explain the background of causal inference and confounding, and show a rudimentary example of this in practice? Because causal inference and confounding are everywhere in healthcare. And the more we understand how great the power of observational data is, the more likely we are to continue to advance the cause of public health.
*A portion of this article is attributed to the writings and lectures of Miguel Hernan, TH Chan School of Public Health at Harvard University




