
As Europe seems to recover from the recent financial crisis, it would be worth sparing a few thoughts for the healthcare situation. As shown by the Euro Health Consumer Index (EHCI), which has been comparing the performance of national healthcare systems since 2005, there has been a steady improvement of key indicators, such as infant mortality, heart fatality, smoking and access to cancer care, to mention but a few. This development has generally been the result of systematic work on policy and delivery levels. The intended outcomes have been achieved in a rational way, helping health systems in almost every country cope with the challenge.
But what is striking when looking into the European landscape is that one essential exception remains: timely access to healthcare services. Here, very different mechanisms seem to rule the performance in Europe, depending on which countries have single-payer health systems. In what are called ‘Beveridge cultures’ – compared to ‘Bismarck’ systems, with multiple payers – waiting for care evidently depends on irrational, unplanned and unintentional but nevertheless devastating cultural factors. It seems that waiting times for healthcare services are a mental condition affecting healthcare administrators and professionals rather than a problem of scarcity of resources.
The ‘waiting times map’
This can be clarified by looking at some of the mechanisms that one would assume to be relevant for waiting times conditions. Take a look at the EHCI 2015 ‘waiting times map’ of Europe. Green indicates good access, yellow shows mediocre performance and red signals significant need of improvement (see Graph A).
As can be seen, long waits can be expected in the UK, Ireland, the Nordic countries, Italy, Spain and parts of the former Eastern bloc. The common denominator is the single-payer system with predominantly tax funding.
But what about other explanations? The money spent, the number of doctors, how care is organised and so forth?
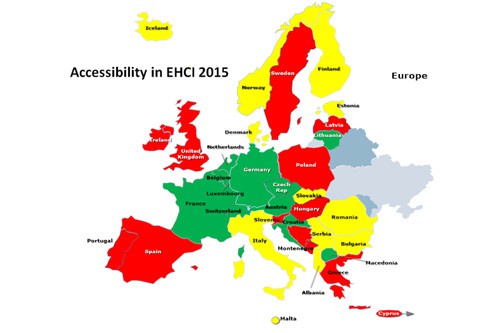
Graph A
Not a matter of money
There is no significant correlation at all between money spent and accessibility of healthcare systems, as is shown in Graph B. This could explain the limited effect of giving billions to NHS or Swedish healthcare to help them reduce waiting times.
As can be seen, there are poor countries spending very little on healthcare (below USD2000 per capita/yr) with the same, or even better, access than wealthy ones, spending three times more. Why is that? Because it is inherently cheaper to run a healthcare system without waiting lists than having waiting lists! Contrary to popular belief, not least among healthcare politicians, waiting lists do not save money – they cost money!
Healthcare is basically a process industry. As any professional manager from such an industry would know, smooth procedures with a minimum of delay or interruption are key to keeping costs low.
There is no significant correlation between money spent and accessibility of healthcare
This brings up the gatekeeping issue – a kind of watershed in healthcare policy. There is a general idea among many healthcare regulators that the patient should not be allowed to directly consult with a medical specialist. The EHCI has measured the outcomes of such policies for more than a decade and, like several other studies, has not found any significant effects of gatekeeping on the level of ambulatory care costs, or on the level or growth of total healthcare expenditure. What the EHCI has found is that GP gatekeeper systems result in waiting time problems for specialist services. Limiting the freedom and choice among consumers comes with a cost.
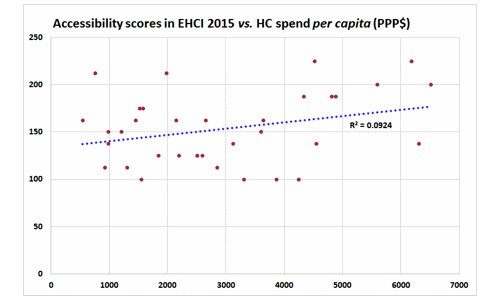
Graph B
Does the doctor see patients – or file statistics?
Further, the number of doctors has very little to do with how long the patient has to wait (see Graph C).
This picture may look somewhat alarming but what it shows is the number of doctors in each country and the number of outpatient contacts a year, ie how often citizens visit a doctor. There is hardly any correlation between doctors per capita and the access to doctors.
The most remarkable conclusion is that in some countries, doctors are highly productive and see a large number of patients. A Commonwealth Fund study of 11 countries in 2012 found that patients were more satisfied with the attention from doctors in countries where doctors see many patients per day. If Swedish doctors were as productive as their Belgium or German colleagues, Sweden would offer good access. And again, there are many more highly productive doctors in the continental mixed-funding, mixed-provision systems than elsewhere.
The economic recovery in Europe seems to have served healthcare well
Continuous access improvement
As initially mentioned, the economic recovery in Europe seems to have served healthcare well. There have, with few exceptions, not been any radical budget cuts on systems levels and the major financial lifeline has been continuous replacement of patented pharmaceuticals by far cheaper generic products. The care production as such has noticed a limited increase of waiting, a tendency made evident by the EHCI annual reports. For elective surgery as well as cancer treatment, a probably austerity-induced slight increase of waiting time was observed for these costly treatments between 2009 and 2013, and a minor improvement in 2014, which continues into 2015. It will be interesting to see if this trend remains during 2016.
The waiting time for major non-acute operations is a vital piece of information, examining the interval between diagnosis and treatment for procedures such as a coronary bypass/PTCA and hip/knee joint replacements. Here the Index cut-off for a green score is a maximum waiting time of 12 weeks.
It is difficult to avoid the observation that, for countries that do have official waiting time statistics (Ireland, Sweden, the UK etc), this in itself can be seen as a negative thing. Countries such as Germany, where waiting times tend to vary in the 2-3 week range, have never felt the urge to produce waiting time data, mainly for the same reason that Singapore has fewer snow-ploughs than Helsinki!
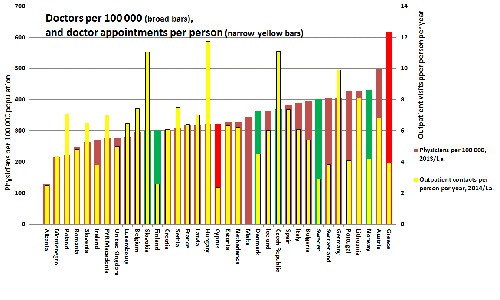
Graph C
CT-scan
As therapy alternatives grow and consumers get more and more anxious to have a correct healthcare diagnosis to learn about their treatment options, services such as a CT scan have become critical. Waiting times for such advanced diagnostics affect not only the chances of quick recovery but also patient satisfaction. To what extent a healthcare system is able to successfully combine medically motivated speed with the kind of quick access that comforts the patient can be looked upon as a useful standard of ‘consumer friendliness’. That is why EHCI indicators compare the time it takes to get a CT scan after the referring doctor’s decision.
The Patient Organisation survey regularly commissioned by HCP (another very useful piece of information, offering a reality check through the eyes of approximately 1,000 patient groups around Europe) provided the distinction between alternatives such as ‘everybody receives an examination within one week’ to ‘everybody waits more than three weeks’. As Graph D shows, in Estonia patients can count on a scan within a week. In Greece patients have to wait longer but – compared to frequent horror stories of the state of current Greek healthcare – access still looks reasonably good compared to the ‘usual waiting time suspects’: the UK, Sweden and Ireland (in this case, joined by half of the countries included in the EHCI 2015 study).
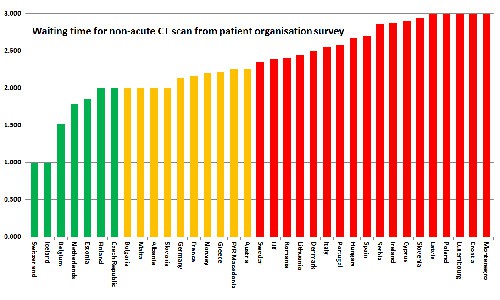
Graph D
What to do with ‘the usual suspects’?
Finally, we end this description of European healthcare accessibility by mentioning the situation in the acute and emergency room in hospitals. It is hardly surprising that the shortest wait (less than one hour) is typically found in Central Europe while the longest wait (more than three hours) again is frequent in countries such as Sweden, the UK and Ireland.
The annual patient review of all access-related indicators in the EHCI accentuates the size and depth of the access dilemma in a number of European health systems, with a focus at the ‘NHS-style’ systems just mentioned. As said initially, long waiting is not a matter of money, number of staff or size of arrows between squares in an organisation’s chart. Rather, what matters is payer-provider relations (‘Bismarck beats Beveridge’), the management status and professionalism (‘NHS-systems are generally overstaffed but undermanaged’) and the organisational ethics (‘Who am I to let people wait longer than absolutely necessary?’).
Evidence speaks volumes. Will the under-performers listen?




