Society is growing, the NHS must meet the needs of an ageing population when staff and budgets are stretched and Brexit is causing uncertainty. In these difficult times, I believe Bayer, and the rest of the pharmaceutical industry, should be partnering the NHS to help provide the support it needs so that professionals can do their jobs effectively and patients receive the best possible care.
Put simply, our role in the past was often limited to researching and developing the products provided to healthcare professionals to treat the patients they look after in surgeries and hospitals. In these changing times, we must go further. We should be pushing ourselves to be delivering more value to our customers that goes beyond the traditional R&D model, enabling the NHS to make the best use of our medicines and its resources.
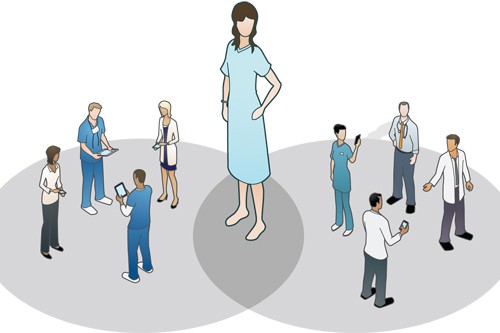
This means working directly with the NHS, on the ground, to meet their local needs. Since 2012, Bayer has been doing this through various joint-working projects – leading the way in our sector. We have a dedicated team working closely with local commissioners and providers to explore ways of delivering better patient care and building quality improvement expertise within the NHS.
Take a recent local NHS partnership aimed at addressing specific access and capacity issues in Southampton. This investment has resulted in a new Mobile Medical Retina Unit launched at Southampton University Hospital which now offers patients living in Hampshire and the South Coast flexible and convenient access to essential treatment, expanding and improving care for people living with a leading cause of vision loss – age-related macular degeneration (AMD). It is only through working closely together with local clinicians to fully understand the problem and identify an appropriate, long-term solution that brings benefits to patients and goes well beyond simply providing a treatment.
We have transformed the way we work with our NHS customers. I am proud to say that there have now been over 30 successful projects within the NHS in the past five years. These include award-winning collaborations that have been recognised as highly competent within the NHS, and as truly innovative and transformational for their way of working and the results they have delivered. Each specific project really is unique.
Our joint working projects are in addition to over 120 current wider collaborations across R&D networks in the UK and Ireland. Improving the use of new and innovative treatments can help reduce long-term health, care and societal costs as they replace traditional, system heavy, in-hospital care and reduce bed days.
I am determined that this continues to be the way that Bayer works with the NHS. Despite the uncertainty and challenges in our environment, particularly related to Brexit, we need to ensure we always keep patients at the centre of what we do.
Need for a balanced PPRS agreement which works for patients, NHS and industry
To allow us to act as true partners to the NHS, it is vital that we are able to deliver that support in an environment that recognises and rewards innovation, not least through a balanced PPRS agreement that works for patients, NHS and the pharmaceutical industry.
We know and recognise that the NHS must manage affordability, increasing the need to provide stable and predictable evaluations and outcomes for all parties. The current PPRS scheme has delivered over £2bn to support the NHS since 2014
The new scheme needs to be balanced to ensure that patients get the new medicines they need; deliver value for money for the NHS; and enable a thriving UK pharmaceutical sector that can continue to innovate in medicines and create jobs and value to the economy.
Reflecting on the experience of the 2014 scheme, there is no doubt that the current agreement has fallen short in fulfilling some of its intended ambitions, particularly around improving access to new, innovative medicines and variability of uptake across the NHS. Right now, the access and reimbursement framework which has evolved in England is challenging, complex, and often duplicative, resulting in patients having slower access to significantly fewer important new medicines. The Government’s own data show those patients in countries like France and Germany are already five times more likely to get access to NICE-approved medicines than NHS patients in England. Medicines spend growth within the PPRS stable at 1.1% (fallen 0.4%) while NHS spend growth is higher at 3.3%.
The PPRS negotiations provide a timely opportunity to consider how routes to market for innovation can be improved as part of a holistic approach to medicines policy and the partnership working I’ve described above. Specifically, this should include building on the recommendations put forward in the Life Science Industrial Strategy and the Accelerated Access Review, to streamline access evaluation processes for new therapies and enable early multi-stakeholder dialogue on potential flexible commercial arrangements, as well as greater accountability for the diffusion and adoption within the NHS.
Bayer, alongside our colleagues in the industry, shares the Government’s vision to ensure the UK becomes the best place in the world to discover, develop and use innovative medicines. Failure to address the underlying issues associated with access, adoption and diffusion of innovation reduces the attractiveness of the UK market which ultimately impacts on patients and the wider economy.
And Brexit is adding to this uncertainty
At Bayer, we are committed to the UK and want to ensure that patients will have a secure access to medicines on day one of Brexit, whether they are on an NHS hospital ward or in another part of the European Union. Like other colleagues in the industry, we are making a significant investment in planning for different Brexit outcomes – money that might otherwise be spent on our partnership working with the NHS.
If the model that we are committed to now and in the future can survive, then we need as little change as possible to ensure the flow of products between the UK, Europe and the rest of the world.
But this needs to happen for all products. Long queues waiting to get in and out of the UK, and a structure that is unable to deal with capacity is simple not feasible. If you take medicines as an example, some have a very short shelf life therefore it is imperative that they get to the NHS and patients in the same timeframes as now.
The bigger picture and our longer term relationships in the context of what is best for patient safety and future innovation, is simply a close regulatory environment. The stronger the regulatory alignment, the more attractive the UK will be for clinical research and excellence both now, and in the future. Regulatory alignment would also continue to ensure that patients in the EU 27 countries benefit from MHRA expertise so the win is clearly on both sides.
If we can achieve this, we will help safeguard an undisturbed medicine supply to patients in the UK and the rest of Europe, supported by common regulatory framework with the EU that supports our medicines and innovation for the future.
Only when we have this, will we be able to provide reassurance to patients and healthcare professionals and together, continue to deliver the innovations and medicines that can enhance and save lives.





