WHITE PAPER: Why do men die younger?
April 12, 2021 | gender health gap, men's health, mental health
It’s a commonly accepted fact that women outlive men. Wherever you live, there’s a good chance that men will die on average eight years earlier than women. Is this an unavoidable fact of genetics or a problem we can begin to solve during the 2020s? We delve into the challenges of men’s health and ask what this means for the healthcare industry. (Originally published March 2020)
This week, we’re discussing men’s health on our social media channels – as an introduction, we wanted to share this edition of MAGNIFI to highlight the key issues impacting men’s health.
In 2019, a review was published by Crimmins et al.3 which aimed to put the gender mortality difference into context. This was achieved through evaluating existing national surveys for data on mortality, disease prevalence and physiological status in order to understand whether men overall have worse health.
Interestingly, the overall conclusion of the study was that while men and women have somewhat different health profiles, these differences are highly dependent on historical time and geographical location.3
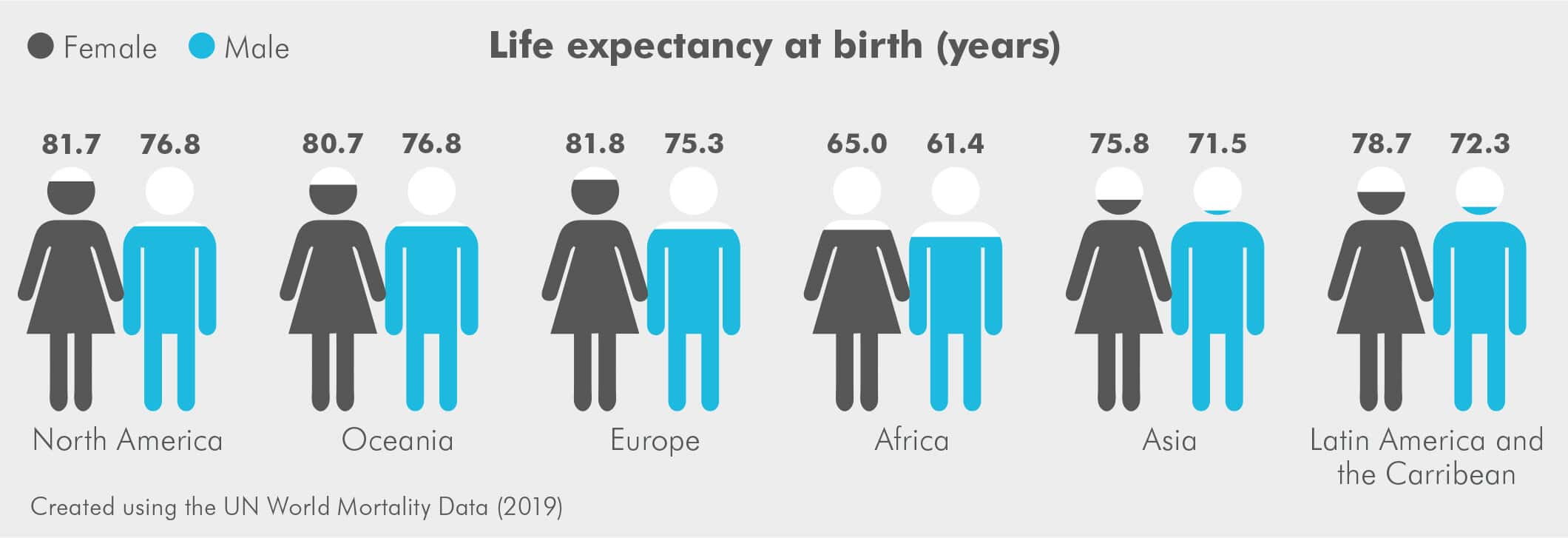
Men were found, on average, to die approximately 6–8 years younger than their female counterparts and have a lower average life expectancy in all countries3
This suggests that factors external to genetics play a role in male health and mortality.
Traditionally, the idea that women live longer has been attributed to the often-riskier lifestyles and occupations of men. However, with the challenging of gender roles over the past few decades, why does this gap show no sign of narrowing?4 And what does this mean for the future of healthcare?
The influence of society
In order to address the gender health balance, it is important to understand the key factors thought to contribute to the problem. Although often dismissed as a result of physiological differences between the sexes, including the lack of the protective effects of oestrogen contributing to heart disease in males, male health isn’t completely predetermined. Many factors contributing to poor men’s health are based on lifestyle.
For example unhealthy habits such as: poor diet, lack of exercise, smoking and excessive drinking are all more prevalent in men.5
Many of the most common health conditions affecting men including coronary heart disease, diabetes and various cancers are also known to be affected by these habits.5
This results in an overall lack of preventative care in comparison to women. Delving even further into the problem raises questions as to why these lifestyle differences in men and women exist in the first place. The main explanation given is that we have been conditioned to act in this way. Traditional gender roles have roots in the evolutionary concept of men acting as providers and women as caregivers. Although these roles are now less strict, they had a big influence on the way our society developed.
The traditional idea of masculinity states that men should be tough, both physically and emotionally.
The masculine gender role also varies based on cultural standards. For example, amongst Russian working-class men, heavy consumption of strong spirits is linked to male status.6
Consequently, 25% of Russian men die before the age of 55 compared with just 7% of British men, which is considered to be predominantly due to the consumption of alcohol and cigarettes.6
Perhaps the most striking influence of the male gender role is on the likelihood to ask for help.
A psychological study carried out in 1989 found that men who expressed traditional attitudes toward the male role were less likely to consult a professional when problems arose with their mental health.7
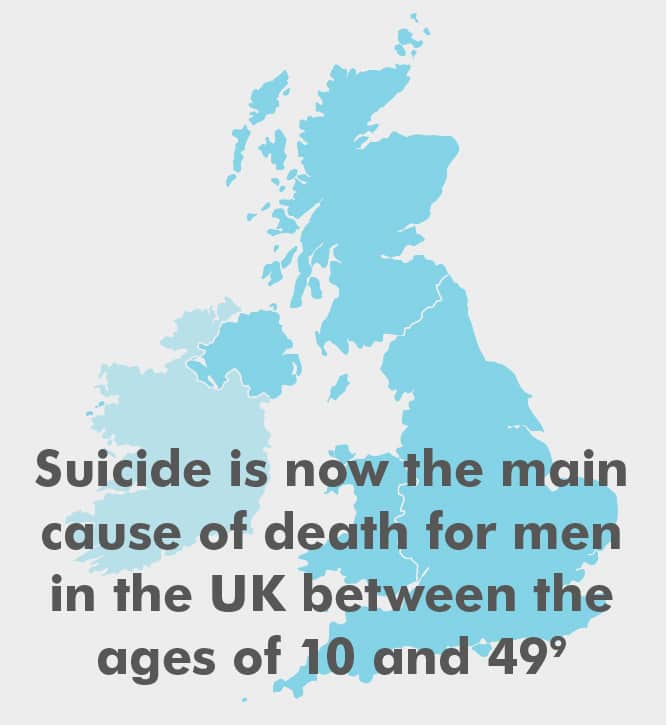
This is most prominently demonstrated by the shocking statistic that three quarters of registered deaths in the UK by suicide are among men,8 with suicide now being the main cause of death for men between the ages of 10 and 49 in the UK.9

A call-to-action
So, what can be done to improve the state of men’s health? There are three main areas thought to be instrumental in making a lasting change to the gender health gap:
Raising awareness – by making the problem more visible, it is hoped that men will learn to identify harmful behaviours in themselves, along with enabling healthcare professionals (HCPs) to better identify warning signs or risky behaviours.

Targeting of healthcare services to men’s needs – be it male-only group counselling sessions or specifically targeted campaigns: it has been demonstrated that a ‘one-size-fits-all’ approach to healthcare is not working. If men aren’t asking for help, maybe HCPs could be the ones to reach out?
Emphasising male proactivity – a cultural movement towards reducing the stigma on seeking help and an ingrained emphasis on a healthy lifestyle could help men adjust to the more preventative emphasis on modern healthcare.

What is being done?
Perhaps the most recognisable stakeholder in men’s health is leading charity, Movember (uk.movember.com). Focussing most of their campaigns around men’s health month in November, this charitable organisation aims to address the key issues in men’s health, in order to make men’s lives ‘happier, healthier and longer’.10 This includes:
- Supporting research efforts for male-specific diseases such as prostate and testicular cancer
- Opening the conversation about mental health
- Addressing the health gap between the genders
Alongside increasing the public profile of men’s health, the proceeds of Movember go towards a range of global projects that aim to innovate the way men’s health is addressed.
Recent projects have included improving HCP’s understanding of eating disorder presentation in men; providing mental health support for fathers following perinatal loss and even ‘MOVE’: a campaign urging men to increase physical activity levels as a way of raising money.

On a local level, individual NHS trusts have addressed the crisis in male health, both by creating a greater awareness for the needs of male patients, but also by drawing attention to the needs of male staff members, particularly in regard to their mental health.11 There are even well-man clinics in place in several hospitals that provide check-ups for some of the most common health issues affecting men.12
However, despite the need to address gender health inequalities being acknowledged by the World Health Organisation,13 Public Health England and the NHS have a distinct lack of mission statements on the topic.
The overall result is a lack of a national cohesive action plan towards the improvement of men’s health in the UK.
The Men’s Health Manifesto created by the Men’s Health Forum,9 calls for increased efforts from all stakeholders: from NHS England, to GPs, to men themselves. Perhaps inspiration could be taken from Ireland, which in 2008 released the world’s first national men’s health policy.14

What can you do?
So, the question is: on an individual level, what can be done within the healthcare industry to effect change? The first and biggest step is to understand the issue. Gaining an awareness of the specific areas in which men are failing to engage with the healthcare system allows you to readdress your approach to male patients in general.
As a HCP, this could range from recognising the subjects on which men are less likely to volunteer information unprompted, to identifying useful new resources for your patients.
From a marketing perspective, it is worth understanding the way in which gender roles affect how information is most effectively communicated.
If men are less likely to seek out help for themselves, then bringing engaging campaigns to them may be the best solution.
A good example of how to creatively market health awareness to men is the ‘Time to Change’ campaign, which promotes mental health awareness in typically male-focused arenas such as through the Football Association and on beer mats in pubs.15
The evidence is there that men and women differ in the way they engage with the healthcare industry and based on the statistics, the current system appears to be more effective for women.
The task therefore is not prioritising male healthcare over female but levelling the playing field so that effective services are provided for both. Although national policy is necessary, there is a lot that can be done on an individual level by those in the industry to address this balance and make the lives of men happier, healthier and longer.

References
1. Barford A et al. Br Med J. 2006;332(7545):808. doi:10.1136/bmj.332.7545.808.
2. Lenart P et al. Sci Rep. doi:10.1038/s41598-019-47111-w.
3. Crimmins EM et al. Clin Chem doi:10.1373/clinchem.2018.288332.
4. Wang H et al. Lancet. Vol 380.; 2012. doi:10.1016/S0140-6736(12)61719-X.
5. Centre for Public Scrutiny. Men Behaving Badly? Ten Questions Council Scrutiny Can Ask about Men’s Health.; 2015.
6. Hinote BP et al. Men Masc. 2012;15(3):292–310. doi:10.1177/1097184X12448466.
7. Good GE et al. J Couns Psychol. 1989;36(3):295-300. doi:10.1037/0022-0167.36.3.295.
8. Suicides in the UK – Office for National Statistics. https://www.ons.gov.uk/ peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/ suicidesintheunitedkingdom/2018registrations. Accessed January 21, 2020.
9. Men’s Health Forum. Men’s Health Manifesto.; 2014.
10. Movember – About Us – The Movember Foundation. https://uk.movember.com/about/foundation. Accessed January 21, 2020.
11. Men’s Health Week, 10-16 June 2019 – Sexual Health Wirral. https://www.sexualhealthwirral.nhs.uk/ support/mens-health-week/. Accessed January 21, 2020.
12. What are well man clinics? – NHS. https://www.nhs.uk/common-health-questions/mens-health/ what-are-well-man-clinics/. Accessed January 29, 2020.
13. WHO Regional Committee for Europe. Strategy on the Health and Well-Being of Men in the WHO European Region.; 2018.
14. Department of Health and Children (Ireland). National Men’s Health Policy 2008–2013.; 2008. www.dohc.gov.ie. Accessed January 29, 2020.
15. Time To Change | let’s end mental health discrimination. https://www.time-to-change.org.uk/. Accessed January 21, 2020.
This content was provided by IGNIFI





